Sernova’s regenerative medicine pouch aims to help millions of people achieve insulin independence.
For George Huntley, 60, living with type 1 diabetes means no two hours are the same. Before every meal, he must measure his blood sugar and decide on a dose of insulin. Any exercise can make his glucose levels become too high or low.
“It’s a rollercoaster of ups and downs,” says Huntley, CEO of the Lexington, Kentucky-based nonprofit Diabetes Leadership Council. “You don’t get a day off.”
If you have diabetes, your pancreas can’t produce enough of the hormone insulin, which regulates blood sugar. Diabetes affects 537 million people worldwide. Ten percent have type 1 diabetes, where the immune system attacks and destroys the body’s insulin-producing cells inside the pancreas. (Type 2 diabetes occurs when the body can’t use insulin effectively, but it can be managed and even prevented with diet and exercise.) People with type 1 diabetes have to monitor their glucose levels and take insulin to control their blood sugar and prevent long-term damage to blood vessels, nerves, and organs. Managing the disease is a daily burden.
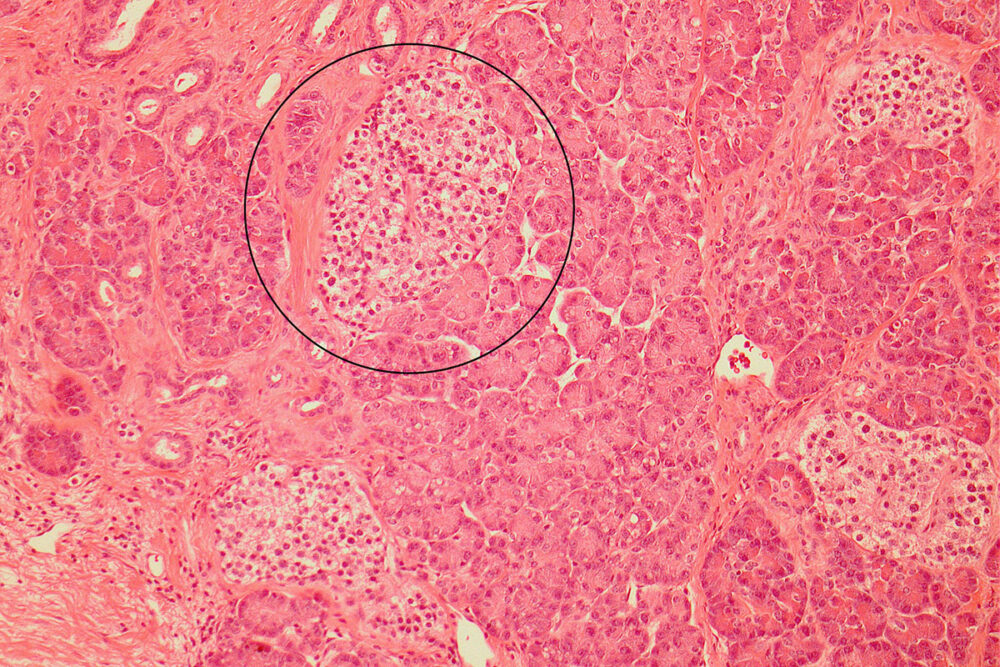
Sernova, an Ontario, Canada-based company at the forefront of diabetes research, wants to change that. They’ve created a cell pouch which is inserted into the belly where blood vessels grow into it. Once that occurs, a surgeon transplants pancreatic islets, into the device. Cells in the islets read a person’s blood sugar and release insulin when needed.
“The cell pouch may act as a potential ‘functional cure’ for a disease that has seen little treatment innovation in recent years,” says Sernova CEO Philip Toleikis.
Current treatments
The past century has seen a number of major breakthroughs in treating type 1 diabetes, with the most recent happening 20 years ago, when University of Alberta surgeon James Shapiro developed the Edmonton protocol, a way of transplanting pancreatic islets from a deceased human donor into the portal vein, which brings insulin from the pancreas to the liver. But inflammatory responses in the blood can destroy a lot of islets, so the effect sometimes wears off, though a review of some 1,500 people receiving islet transplants over its first decade of availability found that 50–70 percent of them were still achieving insulin independence five years after the surgery.
“The only way we’re going to treat millions of patients worldwide is with stem cells.”
Still, the other limitation of islet transplants is that only a certain number of people can benefit from them. Because there is no source of whole pancreases other than deceased organ donors, there are only a limited number of pancreases available in the United States each year. Many of the pancreases that do become available are used in organ transplants already, often given to people who are getting a new kidney. That limits the availability of islet transplantation procedures.
Sernova wants to use the idea of transplanting islets into the body but take it further, using stem cell therapy. Rather than relying on donated organs, they’re working with Hamburg, Germany-based biotech company Evotec, which takes umbilical cord blood, reprograms cells therein back to an embryonic state, and then converts them into insulin-producing beta cells. They are one of several companies chasing an approach like this.
“The only way we’re going to treat millions of patients worldwide is with stem cells,” Toleikis says. But where are they going to put the islets? One option is the portal vein. However, Sernova wants to avoid the inflammatory blood response seen with the Edmonton protocol.
So they’ve created a sack-like device that forms a natural environment for cells to survive and function long term. They place it inside the belly under the skin and once implanted, the patient’s blood vessels grow through the pores of the device and are able to support the growth and development of those beta cells, just like islets in the pancreas are.
Testing
But first, Sernova is testing the cell pouch with human islets from deceased donors rather than stem cells.
In preliminary results of a phase 1 clinical trial involving seven people with type 1 diabetes in Chicago, three people receiving the Sernova pouches produced enough insulin on their own to achieve insulin independence—the treatment threshold at which they could be considered functionally cured of diabetes. “It is wonderful to see the field expanding with different approaches by companies such as Sernova,” says Bernard Tuch, director of the Australian Foundation for Diabetes Research and an expert who is not involved with Sernova’s research. “The data shows [an] improvement in control of blood sugar levels and a reduction in insulin requirements.”
After suffering with type 1 diabetes for 47 years, the first patient has been insulin independent for more than 2 years.
The challenge is getting the dose right. The team placed two distinct portions of islets into the pouch, six months apart, which increased the amount of insulin the patients produced. Then they placed a small dose of islets into the portal vein in an amount that normally wouldn’t have an effect in the portal vein alone. This pushed patients into insulin independence.
Toleikis says that, after suffering with type 1 diabetes for 47 years, the first patient has been insulin independent for more than 2 years. “She had over 21,000 insulin injections, 15 years using an insulin pump, carbohydrate counting, hypoglycemic events, and countless other burdens. She’s now free from that.”
However, Tuch notes that getting to insulin independence required combining the cell pouch system with the standard practice of transplanting islets into the portal vein: “The impressive results have yet to be demonstrated with islets placed in the pouch beneath the skin alone.”
Sernova is doing just that for the second group of patients in their phase 1/2 trial. They are once again using human islets but they’ve increased the size of the pouch by 50 percent so they can insert a higher dose into the pouch alone. They started enrolling patients late last year. It’s all leading up to testing the device with stem cells. They’re projected to start a phase 1/2 clinical trial with stem cells in 2024.
They will continue working with biotech company Evotec, which is creating insulin-producing cells to place in the pouches by manufacturing stem cells from blood or skin cells. “We have worldwide exclusive access to this stem cell-derived technology that can now go into our device,” says Toleikis. “We’re going through the processes with Evotec to scale up the stem cell technology and manufacture the islets, and we’re preparing for clinical trials in 2024.”
Toxic side effects
By moving the device from the portal vein in the liver to the stomach, Sernova has addressed the inflammatory response from the blood. However, they haven’t yet been able to prevent immune cells from attacking donor islets. So people who have received the pouches so far have had to take anti-rejection drugs to keep them viable. Those drugs reduce kidney function in some people and can also increase the risk of infections and sometimes cancer, though that’s rare.
Sernova is working on a polymer coating for the pouch to protect the cells from an immune attack and looking into gene editing stem cells to make them less visible to immune cells.
Other companies are also working on transplanting islets. San Diego-based regenerative medicine company ViaCyte is more advanced, as they’ve started using stem cell-derived technology in an initial trial. One potential advantage Sernova has is that they’re using stem cells derived from blood rather than embryonic stem cells like ViaCyte and others, which means their device can be used in countries and for people who won’t use embryonic-derived technology for legal or ethical reasons.
The progress of Sernova and its competitors
Commercialization
The team hopes to not only provide a viable alternative to insulin injections, but by doing so, reduce diabetes-related complications, like heart disease, blindness, and amputations.
This would reduce the total cost of diabetes. Toleikis explains, “The insurance companies said they’d pay $200,000–$400,000 for each treatment if we could make it work for two years. It sounds like a relatively large number, but with hospital visits and side effects going down, it’s a major improvement to the health care system in terms of cost.”
“Having a working set of islets is the holy grail.”
Sernova also intends to test their cell pouch technology for other indications—to deliver therapeutic cells to people with hemophilia A or people who have had their thyroid glands removed. So far, they’ve conducted successful preclinical trials in mice.
As for their progress in treating diabetes, Huntley is optimistic. Even though he was not part of the trial, he has been following it closely.
“Everyone wants this to work. Having a working set of islets is the holy grail. But it’s got to be without immunosuppressants. I’ll be first in line if they succeed.”
Editor's note: This story was updated on 2/24/23 to correct the name of the Australian Foundation for Diabetes Research and to clarify in the fourth paragraph how insulin is released from the pouch.








