Inspired by Arctic fish, scientists are developing frost-fighting methods to keep organs viable for as long as possible.
Imagine a strawberry, red and ripe, tucked into the freezer, or a head of lettuce accidentally frozen in the fridge. Then picture it days later, defrosted. It’s a mushy, unappealing mess. Now you roughly understand the challenge that organ transplant teams face every day keeping tissues fresh. Organs, like produce, don’t freeze well. The slightest bit of crystallization can burst cells, rip veins, and render a precious, carefully salvaged heart, lung, or kidney unusable.
Yet keeping organs cool is critical to maximizing their usable lifespan, keeping them viable for lifesaving organ transplant surgeries which often take place in another hospital if not another state.
The United Network for Organ Sharing is in charge of matching organs with potential recipients in the United States. Despite reports that 2022 was a record-setting year for liver, heart, and lung transplants, there are still far more people in need of a transplant than organs available. About 104,000 people are on a waiting list for transplants in the United States right now, with just under 60,000 of those people immediately eligible to receive an organ based on the severity of their illness. Some 42,000 transplants were completed last year. But roughly 6,000 of those eligible for transplant, or 17 people each day, will die this year while waiting for their new life-saving organ, according to government data.
Regardless of eligibility, when it comes to transplants, even a short delay can prove deadly.
Organs have just hours of viability once they are removed from living or dead donors. Under ideal conditions, a heart or lung currently has 4–6 hours, livers have 8–12, and kidneys have up to 36 hours of viability outside the body. Cooling organs helps preserve them, but it can also lead to the formation of ice crystals that damage delicate tissue, ruining donated organs. Now, a spate of startups are working on new ways to safely cool organs for longer and at lower temperatures.
“We are basically going through a revolution in transplantation.”
“We are basically going through a revolution in transplantation,” says Korkut Uygun, a biomedical engineer and expert in organ preservation at Harvard Medical School. “There will be many devices, many protocols, many companies that compete.” Uygun expects a range of products targeted to specific organs, or specific transportation or storage needs, in the coming years, thanks to an influx of research dollars and new technology.
Chemist Xiaoxi Wei and her one-time classmate at the State University of New York at Buffalo, Mark Kline, hope to be among them. After graduate school, the two launched X-Therma, a cell, tissue, and organ preservation startup, back in 2015. Their goal was to develop a new generation of living medicine, whether through cell-based therapies or cryopreserved organs. It’s Wei’s brainchild, and she’s spent the past eight years talking to potential funders, supporters, employees, and, more recently, the FDA.
Wei’s story starts with a beloved grandfather, who died while waiting for a liver transplant when she was 8. Heartbroken, Wei vowed to find a way to bank usable organs for future patients. The story is still unfolding today.
Dimethyl sulfoxide (DMSO) is the standard chemical cryopreservative for cells. But for organs, the amount of dimethyl sulfoxide required for cryopreservation is difficult to diffuse evenly. Even when used to cryopreserve cell-based therapies, it can cause harmful side effects. Scientists are testing different methods of washing it away and trying different transplant procedures and transport devices. But it’s been tough to challenge long-established procedures.
“All of these things have complications, and current protocols are sticky,” says Marcus Muench, a hematologist at San Francisco’s Vitalant Research Institute who collaborated with Wei to validate an early X-Therma cell cryopreservative called XT-Thrive. “Nobody wants to change anything that’s mostly working.”
Wei first developed the XT-Thrive product as an alternative to dimethyl sulfoxide. Its secret ingredient is a peptoid—a biological molecule that mimics the structure and function of proteins found in nature—that Wei created, inspired by Arctic flounder and other fish. Fish living in these frigid waters have special proteins that act as a natural antifreeze to keep their blood flowing.
The proprietary cryopreservative, which she describes as “DMSO-, protein-, and serum-free,” performed as well as a mixture of 10 percent dimethyl sulfoxide and serum (a common cryopreservative) in mice stem cell transplants in a 2021 study. But Wei has her eye on a bigger target: whole human organs. And cryoprotectants that work for cells typically won’t work on organs.
“The amount we have to use to prevent a freezer burn is so large it actually will really hurt the organ and will kill the organ with toxicity,” Wei says. “We need to find a new molecule that is hyper effective to control ice formation, which requires a very low concentration to do the job and does not introduce toxicity—and that does not exist in the world.”

From the cooler to the chest freezer
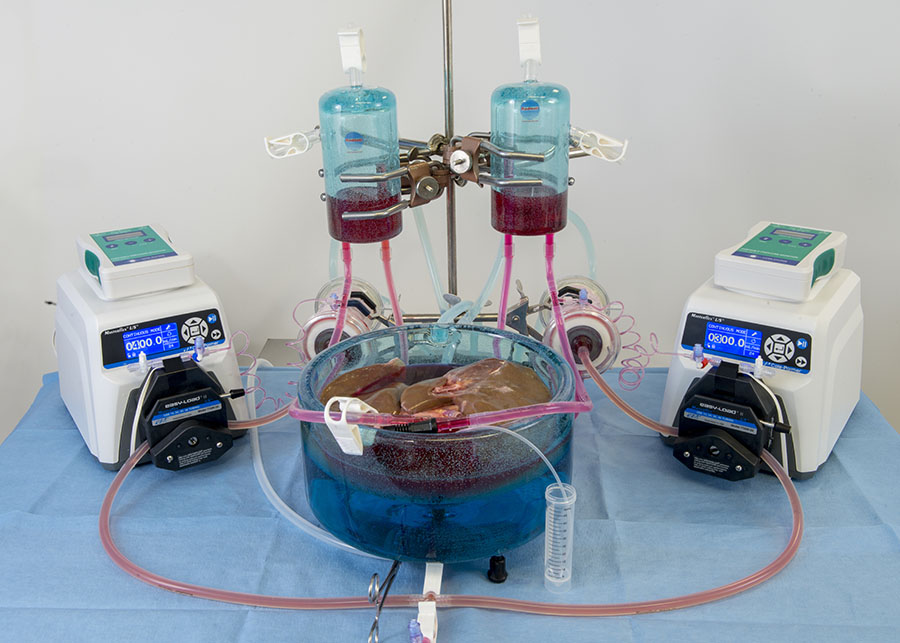
A chemical compound that limits ice crystals in cooled organs for transplant is just one potential solution. There’s also an otherworldly process called ex vivo perfusion in which machines are connected to the organ that mimic the environment, nutrients, and processes normally found inside the body. This can buy time for transport or someday could even give a potentially less-than-stellar organ the chance to heal before being transplanted, increasing the supply of viable organs for people in need. (Imagine, in the future, a lung recovering from pneumonia after it’s removed from the donor.)
A combination of ex vivo perfusion, supercooling, and chemical cryoprotectants is another possibility, and one that’s shown promise in human livers.
Not every type of cryopreservation is the same, though it always involves very low temperatures. The coldest is deep cryogenic storage, which can mean temperatures down to -196° C, the temperature of liquid nitrogen. An organ could theoretically be preserved for years and years at this temperature. And the colder an organ can be safely stored, the longer it will last. But the coldest temperatures bring their own challenges: Ice crystals can form even on rewarming, and longer, colder processes require more cryoprotectants, which can be toxic.
Deep cryogenic storage is “all about shepherding an organ or biological material through this very harsh journey down to liquid nitrogen temperatures and back up,” says Jedediah Lewis, CEO of the Organ Preservation Alliance, and an advisor to X-Therma competitor Sylvatica. “Organ preservation in a high subzero, high subfreezing temperature range, that’s kind of like making part of the journey and then coming back.”
Startups like X-Therma and another competitor, Edmonton, Alberta-based PanThera CryoSolutions, are seeing promise working in high subzero temperatures, a range in the ballpark of -5° to -30° C. Following a strict definition, these aren’t cryogenic temperatures, which typically go down to -80° C, but startups commonly use the cryo- prefix, a nod to working in the subzero realm. With a shorter path from procurement to cooling to transplant than deep cryogenic storage, startups and scientists alike hope technologies in high subzero temperatures will replace procedures used in today’s viable organs, which are preserved in coolers on ice.
Arctic inspiration
Back in the lab, thinking about her grandfather, Wei developed a new solution, XT-ViVo, based on that same specially formulated peptoid inspired by proteins found in Arctic fish. Because it is effective in low concentrations, scientists at X-Therma began testing it on kidney transplants in pigs. Surgeons flush donor kidneys with the new solution, a simple swap for the dimethyl sulfoxide currently used.
“The idea itself of using such peptoids sounds very promising,” Uygun says, pointing out that proteins often cause reactions and can be distributed uniformly in cells and organs.
But Wei isn’t the first chemist to be inspired by Arctic fish. Jason Acker, a co-founder and senior research scientist at PanThera, says he’s years ahead of X-Therma, at least where cell cryopreservation research is concerned. The company’s synthetic, carbohydrate cryopreservative was inspired by antifreeze proteins in winter flounder and northern Atlantic cod. It was first used paired with glycerol to cryopreserve red blood cells, and is now being used alongside dimethyl sulfoxide to cryopreserve immune cells.
The outcomes of research like Wei’s and Acker’s include better cryopreservation for personalized, cell-based treatments. Personalized cancer therapies, like using CAR T cells, or genetically altered T cells that target tumors, can cost hundreds of thousands of dollars. There are similar therapies that don’t require a personalized approach, but these are difficult to cryopreserve. PanThera’s carbohydrate compound addresses this, Acker says, allowing cells to be stored at lower temperatures with less damage and increasing the number of usable cells that survive the freezing and rewarming process.
“You’ll hear companies claim that, ‘Ninety-eight percent of our cells are recovered from the cryopreservation process.’ Well, that means they’re there and you can physically count them, but they’re not functional. They’ll go on to die within 24 hours,” he says.
With PanThera’s cell-based cryopreservative already on the market, Acker plans to expand to organs, “challenging some of those assumptions around what causes damage,” he says.
Meanwhile, pig kidneys using X-Therma’s system can potentially be transplanted up to 120 hours after they are procured. And Wei is already thinking far beyond organ transplant, to the possibility of preserving vaccines, and a host of futuristic medical advances.
“You can consider us like golden shovels for all living medicines,” she says, referring to the ceremonial tool used at a groundbreaking. Wei’s peptoid-based solution, plus an organ-carrying device, won a breakthrough device designation from the FDA, but is still at least a few years away from FDA consideration for human use.
Like X-Therma, Acker is currently in the midst of testing his organ cryopreservation method in animals. But he ultimately expects that surgeons will use an approach that combines a handful of the biotech approaches in development today. For example, ice crystals can form during the rewarming process as well, so scientists are working on microwave and magnetic heating to find speedier warming methods.
“This is the first detailed protocol describing how to perform subzero preservation of human organs.”
“In a theoretical world, if you could cool down and warm up instantly, then you wouldn’t have to add chemicals. But we don’t have the technology to do that,” says Saffron Bryant, a researcher at the Royal Melbourne Institute of Technology in Australia, who specializes in cryoprotectants for mammalian cells. This means that simply cryopreserving organs is just one part of a complex equation.
Elsewhere, supercooling is being tested on human organs outside the human body. At North Charleston, South Carolina-based Sylvatica Biotech, Uygun’s technique for supercooling livers is under development. It involves procuring a liver from a human donor (in experiments, researchers used organs unsuitable for transplant). The liver is flushed with a special preservative solution before it’s placed in an airtight bag, then cooled to -4° C.
This combined protocol allows organs to be stored below their freezing point without ice crystals forming. In a 2020 study, the process extended the life of a human liver by 27 hours, a leap forward. “To our knowledge, this is the first detailed protocol describing how to perform subzero preservation of human organs,” Uygun and his colleagues wrote.
Sebastian Giwa, Sylvatica’s founder and CEO, says the company’s current progress is under wraps as they attempt to bring this technology to market. But the perfusion platform itself could potentially be used for organ healing post-procurement, he says. For example, while Sylvatica is focused on liver research, elsewhere “they can actually have enough time on the pump to cure the lungs from pneumonia.” It would be very risky otherwise, Giwa says, to transfer lungs from a person with pneumonia into immunosuppressed people.
Fresh funding draws cryobiologists
Despite research underway and high-profile experiments like the one in 2022 where a dying human volunteer received a pig heart, procedures for preserving organs for transplant haven’t changed much in recent years. “We’re still doing the exact same thing as was done 60 years ago,” says transplant surgeon and scientist Gerald Brandacher, who also serves as a medical advisor for X-Therma. It’s partially due to funding.
Developing new chemical compounds for cryopreservation has a price tag potentially in the millions. Though it will likely still cost less than, say, drug development, successful organ cryopreservation is just one part of a multi-step transplant process that includes transportation and rewarming. Yet large-scale, collaborative research is still rare, Lewis says, though there are millions more in funding being awarded today compared to five years ago.
Acker estimates there are just 300–400 cryobiologists in the world, and a large fraction of those are engaged in unrelated fields, like agriculture, working on food preservation upgrades like eliminating freezer burn. Yet, with a growing number of cryobiologists interested in biomedical science, progress is quickening.
And organ procurement failures in the United States have already grabbed national attention, as Congress assembled a task force in 2021 to address abnormally high rates of waste and mismanagement. With timelines uncertain—a lack of funding, or clinical trial mishap could derail even the most promising technology—the path forward is sometimes murky.
Yet somewhere deep under the Arctic ice is a fish that holds the secret to keeping donated tissue viable longer. And somewhere else, in a lab, a once-unviable organ is being carefully flushed, cooled, protected, and preserved. Meanwhile, tens of thousands of people are anxiously waiting.