Targeting a key molecule that helps the brain process sensory threats could lead to new treatments for PTSD, migraines, and autism.
Imagine crossing a busy street in Manhattan at rush hour while yammering on your cell phone. The lights change, the engines roar, and you look up from your call to suddenly find yourself thrust onto the middle of Fifth Avenue with a wall of taxis bearing down.
For a fleeting moment, you feel everything: The sounds of blasting horns, the lumpiness of the pavement, a metallic taste in your mouth, that awful smell of standing over a sewer vent, and the feel of your cell phone as it slides away from your ear just before you panic. Run!
All the fear in your brain runs through a thumb-sized, almond-shaped chunk of tissue called the amygdala. It serves as the brain’s surveillance hub for processing sensory threats, such as when we see someone displaying hostile body language or the looming rush of oncoming traffic. The amygdala is like the switchboard and switchboard operator all in one: It helps us detect threats around us, processes the fears and other emotions that these threats (real or not) elicit in our brains, and signals a five-alarm fight-or-flight response to our minds and muscles.
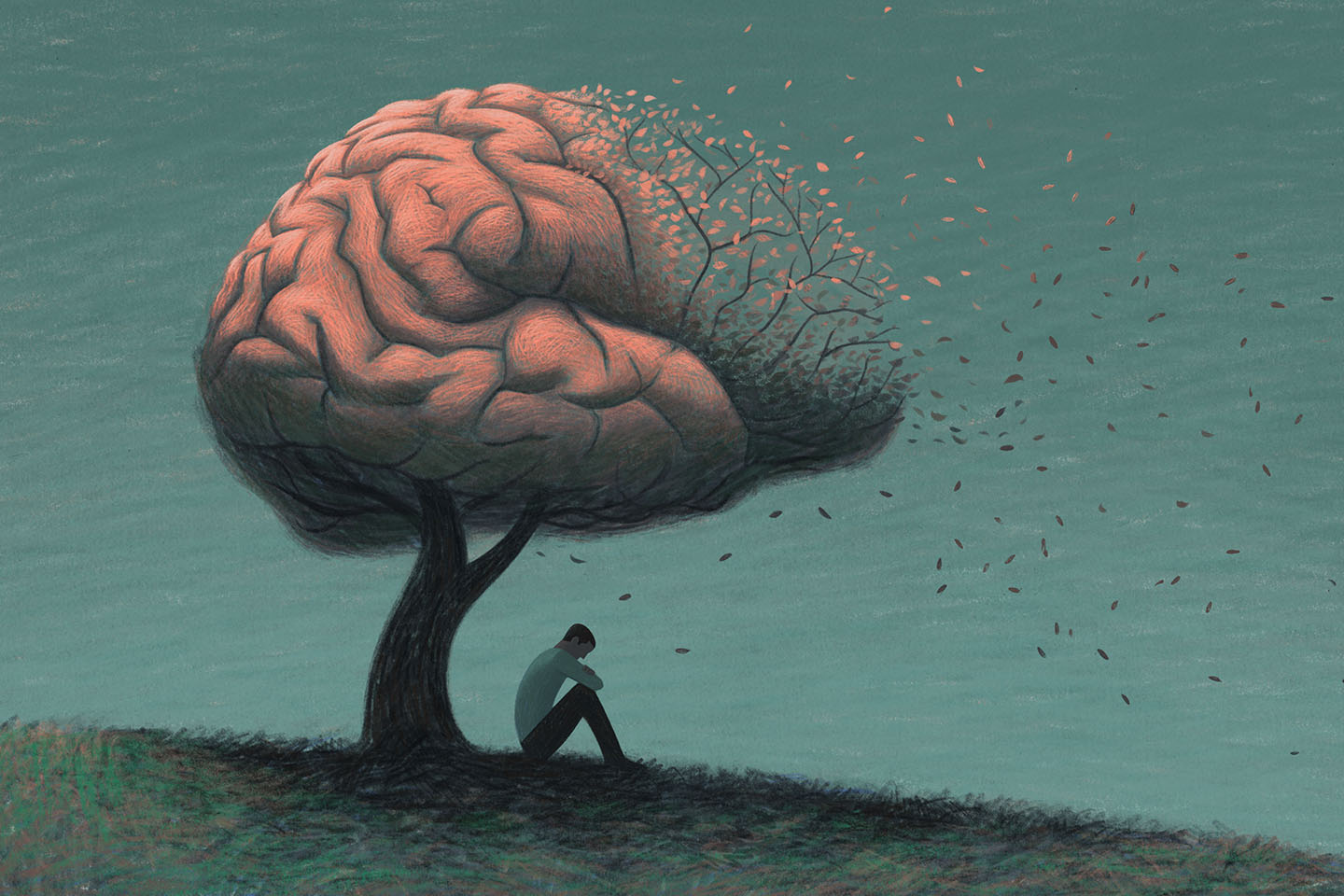
The amygdala is also the part of the brain involved in the formation of fearful memories, which is an essential evolutionary adaptation that helps us survive through learned behavior but also plays a role in post-traumatic stress disorder (PTSD), a mental illness triggered by either experiencing or witnessing a terrifying event.
Yet for all neuroscience knows about what the amygdala does, exactly how it goes about processing fear and turning simple sensory cues into emotional alarm bells is not entirely clear. Part of that mystery has been explained this week by scientists at the Salk Institute for Biological Studies in La Jolla, California. They have uncovered a key molecular pathway in the brain that distills threatening sights, sounds, and smells and tells us to be afraid (be very afraid).
“Although it was thought that a single pathway that integrates all these cues would be beneficial to survival, no one had ever found such a pathway, says Sukjae Joshua Kang, a co-author of the study. “We discovered the pathway.”
In a study published August 16 in the journal Cell Reports, the Salk researchers finger a tiny protein found in the brain called calcitonin gene-related peptide (CGRP). They found that in the mouse brain, two distinct populations of CGRP neurons—one in the thalamus, one in the brain stem—project to non-overlapping areas of the amygdala, assemble multiple sensory cues into a unified signal, imbue that signal with the appropriately negative weight of danger, and convey a strong threat warning to the amygdala, which enables the animal to respond quickly to perceived threats.
The CGRP circuit “acts as a central alarm system for the brain by relaying negative sensory cues from all five senses (sight, sound, taste, smell, and touch) to the amygdala,” Kang says. “Additionally, we found that the same pathway is critically involved in fear memory formation.”
While mouse brains are much less complex than human brains, they share common mammalian features and chemistry, and the same mechanisms as people. The same neuro regions also abundantly express CGRP in humans as well, for instance.
Our brains’ central alarm system
The discovery of this unified sensory pathway combining sensory threats from all over the brain and relaying them to the amygdala demonstrates exactly how the brain achieves what so many neuroscientists suspected it did for many years. Previous research has long shown that while many different pathways independently relay sound, sight, touch, and other potential “danger” cues through multiple brain regions, somehow the amygdala receives this heavy input in parallel—all at once. Nobody knew how the brain achieves this bundling of signals, but the Salk team found that neurons having the neuropeptide CGRP do the job.
Kang says now that the specific brain circuits that transform negative sensory cues into fear have been discovered, that basic discovery could suggest ways to quiet fear or its effects by developing “antagonist” drugs for people suffering PTSD or hypersensitivity disorders such as autism. “The next step is to find antagonists, therapies that will help quiet the circuit when it is acting abnormally, while preserving its key role in ‘real’ dangers such as a fire or flood,” Kang says.
When asked what fear—such as what one experiences during a fire—has to do with illnesses such as fibromyalgia or autism, Kang says, “hypersensitivity disorders, migraines and autism, and chronic pain disorders such as fibromyalgia, are not caused by fear.
“Our study could serve as an anchor to use this kind of drug in relieving threat memories in PTSD or sensory hypersensitivity in autism.”
“However, like any alarm system, if it malfunctions [that] can lead to false alarms,” Kang says. “People with those disorders perceive otherwise normal sensory cues as threats, and since hypersensitivity disorders can affect memory, finding ways to quiet the sensory overload by manipulating the alarm circuit is important.”
Kang is specifically interested in the role that CGRP neurons play in migraines. “Although we have not tested it yet, we know that migraine episodes might be associated with the activation of the CGRP neurons in the thalamus and brain stem since they are triggered by sensory cues. And since drugs that block CGRP have been used to treat migraines, our study could serve as an anchor to use this kind of drug in relieving threat memories in PTSD or sensory hypersensitivity in autism also.”
Commenting on the study, Amit Etkin, the founder and CEO at Alto Neuroscience, who was not involved in the research, says: “Kang and colleagues conducted an elegant set of studies showing that neurons within the amygdala that signal using the CGRP peptide are critical for tying together information from different senses into a ‘whole experience’ in the context of threat.”
Etkin cautions that the study was done in mice and of course work in animals often translates poorly to humans. Nevertheless, he says the involvement of CGRP raises an intriguing possibility because there are already existing drugs targeting it on the market.
“Blockers of CGRP have been recently developed as effective treatments for migraine,” he says, which include both monoclonal antibodies and traditional small molecule drugs. “Thus, it may be possible to study the clinical effects of blocking CGRP in humans, which affords a rare opportunity to test basic science to human clinical trial translation relatively quickly.”